In response to the disparities, which are particularly stark for American Indian and Black Minnesotans, officials are investing millions of dollars from the opioid settlement in culturally specific treatment programs.
Farhia Budul knows the devastating effect of opioid addiction. As a Somali woman in long-term recovery, she’s made it her mission to help others, especially in Minnesota’s East African and Muslim communities, overcome it as well.
“You can just see problems and people struggling with addiction in plain sight,” she said.
The opioid epidemic, fueled by a surge in fentanyl use, has shattered thousands of families across Minnesota. It has hit hardest among the state’s people of color, who die at disproportionately high rates when compared with white Minnesotans.
American Indians were 12 times more likely than whites to die of an opioid-involved overdose in the state in 2022, while Black Minnesotans were four times more likely to die, according to preliminary data from the federal Centers for Disease Control and Prevention.
“[Opioid] overdose is an issue for the whole state of Minnesota,” said Pearl Evans, a prevention program administrator for the state Department of Health. But, she said, “the African American and the American Indian [communities] are the two racial groups that have the highest disparity. So those are our priorities to really reduce the burden on those two communities.”
In response, cities, counties and the state are pouring millions of dollars into culturally specific treatment programs, using money from national settlements in cases against opioid makers and distributors over their role in the crisis. The state Department of Human Services said it licenses 55 such programs.
Hennepin County allocated $8.8 million in opioid settlement money over two years to 41 culturally specific programs that fight opioid addiction and address systemic disparities. The focus is on African American, American Indian, East African communities and unsheltered homeless populations, county officials said.
The city of Minneapolis, which accounted for approximately a quarter of all opioid-related deaths in the state in 2022, has recently awarded nearly $374,000 to five community based organizations with the aim of increasing access to and options for treatment, recovery and prevention, particularly targeting underserved communities and youth.
“It’s a scary time right now,” said Lolita Ulloa, Hennepin County’s director of system design. “But really the sense of what is going to change is really based on the community.”
The county and state also are pushing efforts to gather additional race and ethnicity data to better identify needs and improve community engagement with inclusive language and better access to Naloxone, a drug that reverses opioid overdoses.
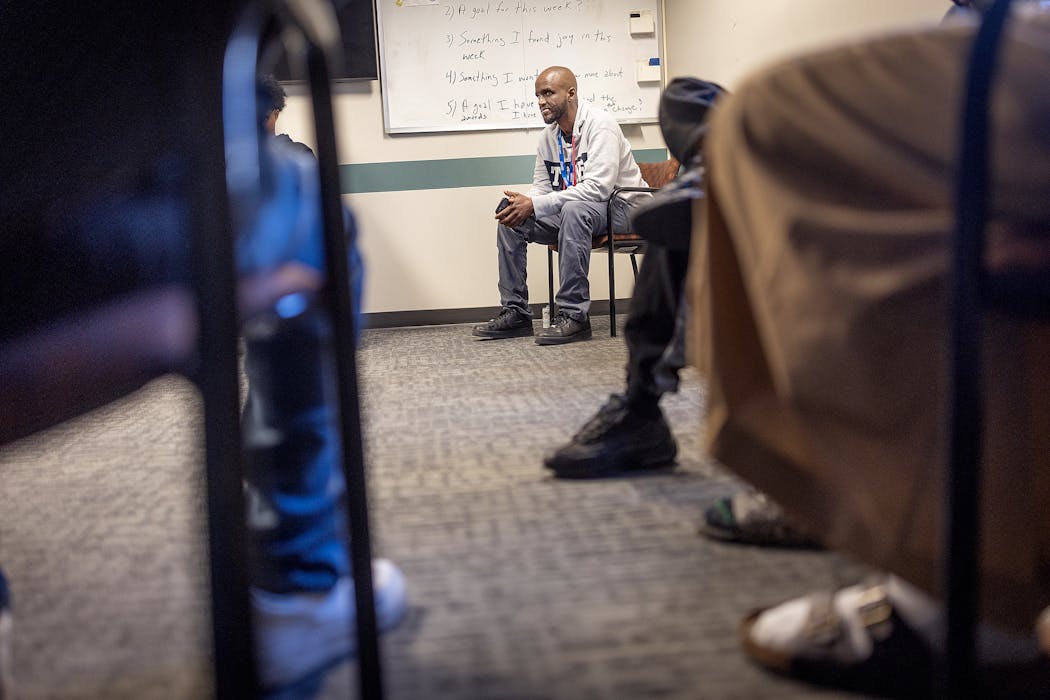
Lori Wilson, CEO of Turning Point, a longtime provider of culturally specific substance use disorder treatment for African Americans on Minneapolis’ North Side, said opioid abuse “has been devastating.”
Wilson said one of the barriers to treatment for people of color is “cultural mistrust” of health care professionals. That’s where organizations like Turning Point, which has Black leadership and staff, can offer a sense of safety.
“If I have an opioid problem,” Wilson said, “it’s unlikely I’m going to take it outside my community.”
‘At war with fentanyl and opioids’
Sharyl WhiteHawk is an enrolled member of the Lac Courte Oreilles Band of Lake Superior Ojibwe in Wisconsin and an addiction counselor at Khunsi Onikan Treatment Program at the American Indian Family Center in St. Paul.
She and others who work in the field point to the long history of persecution — American Indians killed and pushed off their land by European settlers and forced erasure of language and culture at boarding schools — that has reverberated through generations.
“What makes us much more vulnerable to overdose deaths is that we have so many layers of unresolved trauma and unresolved grief,” she said. “Because of the boarding school experience, the only coping skill that has been passed down is don’t talk, don’t tell and don’t feel.”
As a result, American Indians involved in treatment programs say that a key to recovery is reintroducing the Native culture, including traditional ceremonies, and spirituality. For instance, a cedar healing ceremony uses traditional cedar medicine to wash away unresolved grief and trauma.
“Our cultures are a way of life, and our teachings show us how to be good human beings and in harmony with our creator,” said Kateri Coyhis, an enrolled member of the Stockbridge-Munsee Community Band of Mohican Indians in Wisconsin and executive director of White Bison, a Native American nonprofit based in Colorado Springs. The organization provides culturally based programs and resources primarily geared for recovery from alcohol and substance use throughout the United States and Canada.
“I feel we’re at war with fentanyl and opioids,” said Stephen Montry, a licensed alcohol and drug counselor in the Twin Cities area and an enrolled member of the Cheyenne River Sioux Reservation in South Dakota. Montry, a descendant of the White Earth Ojibwe Nation, lost a nephew to a fentanyl overdose in 2022.
“We need to get at the root — why we’re stuck in these patterns,” he said.
Overcoming stigma to find support
From 2018 to 2022, 45 overdose deaths were recorded in Minnesota’s Somali community, according to the Health Department. But state health officials caution even this number is an undercount.
The Minnesota Somali Community Center tries to track opioid overdose deaths with the help of Janazah Project MN, a Facebook page run by the funeral director of the Garden of Eden Islamic Cemetery in Burnsville. The community center said there were as many as 13 opioid related deaths in January 2024.
“We are dealing with a crisis that we have never seen before and it’s devastated almost every family in our community,” executive director Hassanen Mohamed said.
Islam strictly prohibits the use of drugs, alcohol and other mind- and mood-altering substances, leading many Muslims to suffer in isolation and making the opioid crisis a “silent killer” in the East African Muslim community, Budul and other Somali professionals say.
Many families avoid reporting deaths as an overdose, instead attributing them to other causes, such as heart attacks and dying in sleep, to keep them out of official records. Some decline autopsies and toxicology tests, which would reveal those deaths, citing religious exemptions.
Budul is trying to address those challenges through her Niyyah Recovery Initiative. The nonprofit offers a blend of more culturally sensitive and faith-based approaches, including the first Islamic version of a 12-step program in Minnesota.
The program, Millati Islami — meaning “the path of peace” — was founded in Baltimore in 1980s to assist Muslims struggling with addiction find healing, support and guidance within the framework of Islam. The Minnesota chapter hosts Zoom discussions with its more than four dozen members at least three times a week.
“We need that cultural component, which really involves our spirituality, and connecting us back to Allah,” said Budul, who also often shares her own story of battling addictions and shame to instill hope in others.
Meanwhile, at the Alliance Wellness Center in Bloomington, founder Yussuf Shafie grows frustrated as he reviews client files. He said he knows the available state-level data on opioid overdose in the Somali community doesn’t match the sad reality.
“I went to many funerals that I cannot even count,” said Shafie, a social worker. “How does a 22-year-old or 24-year-old die in their sleep? I mean, people die all the time, but the story doesn’t add up. There’s just a lot of shame and stigma.”
The center recently expanded its services by adding eight beds for Muslim and East African women with opioid use disorder. It’s one step, he hopes, in fulfilling a longstanding need.
Data editor MaryJo Webster contributed to this story.