- August 2024
- BMC Primary Care 25(1)
- 25(1)
DOI:10.1186/s12875-024-02483-5
- License
- CC BY 4.0
Authors:

Download full-text PDFRead full-text
Download citationCopy link
Abstract and Figures
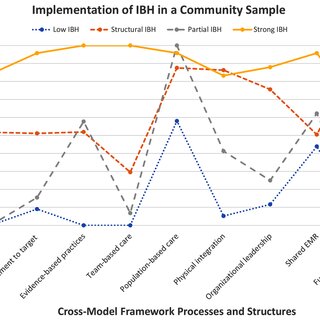
Background People with diabetes, vascular disease, and asthma often struggle to maintain stability in their chronic health conditions, particularly those in rural areas, living in poverty, or racially or ethnically minoritized populations. These groups can experience inequities in healthcare, where one group of people has fewer or lower-quality resources than others. Integrating behavioral healthcare services into primary care holds promise in helping the primary care team better manage patients’ conditions, but it involves changing the way care is delivered in a clinic in multiple ways. Some clinics are more successful than others in fully integrating behavioral health models as shown by previous research conducted by our team identifying four patterns of implementation: Low, Structural, Partial, and Strong. Little is known about how this variation in integration may be related to chronic disease management and if IBH could be a strategy to reduce healthcare inequities. This study explores potential relationships between IBH implementation variation and chronic disease management in the context of healthcare inequities. Methods Building on a previously published latent class analysis of 102 primary care clinics in Minnesota, we used multiple regression to establish relationships between IBH latent class and healthcare inequities in chronic disease management, and then structural equation modeling to examine how IBH latent class may moderate those healthcare inequities. Results Contrary to our hypotheses, and demonstrating the complexity of the research question, clinics with better chronic disease management were more likely to be Low IBH rather than any other level of integration. Strong and Structural IBH clinics demonstrated better chronic disease management as race in the clinic’s location became more White. Conclusions IBH may result in improved care, though it may not be sufficient to resolve healthcare inequities; it appears that IBH may be more effective when fewer social determinants of health are present. Clinics with Low IBH may not be motivated to engage in this practice change for chronic disease management and may need to be provided other reasons to do so. Larger systemic and policy changes are likely required that specifically target the mechanisms of healthcare inequities.

Figures – available from: BMC Primary Care
This content is subject to copyright. Terms and conditions apply.