Since the White House announced this “historic public-private partnership,” 63 sites have opened nationwide. Just eight are in black neighborhoods.

Adarra Benjamin, a 26-year-old black home care worker in Chicago, lacks the luxury of staying home during the Covid-19 pandemic. She assists several elderly patients. Her work demands travel by public transit. Her duties — picking up groceries, running to the post office, counseling clients — have, amid the news of death and disease, devolved into a series of anxiety-inducing tasks.
“I am afraid because my job consists of me not only going in and out of someone else’s home, but shopping for other people,” she said. “It just feels like panic.”
Adarra remains at risk as an essential worker. Chicago stands flush with coronavirus. Cook County, which includes Chicago, has the sixth-most cases of all counties in the country, according to a New York Times tracker, as of April 27. The virus continues to ravage the city’s predominantly black South Side, where Adarra lives with her mother. Recently, when Adarra’s cousin exhibited symptoms of Covid-19, particularly difficulty breathing, he struggled to obtain a test, going to the hospital twice before he received one testing positive.
The situation rattled Adarra. “It has honestly, like, put me into fear,” she said. “To know he went there and that they didn’t have a test to take immediately pushes me back, like, ‘Okay, maybe I could do more harm by going to get tested than I would just staying away.’”
“So now I am really confused as to should I get tested,” she said. “Do they even have enough tests?”
Local activists, politicians, and city data echo the concern about equitable access in Chicago. According to the Chicago Department of Public Health, black people in Chicago make up a majority of Covid-19 deaths, at 56 percent, as of April 26.
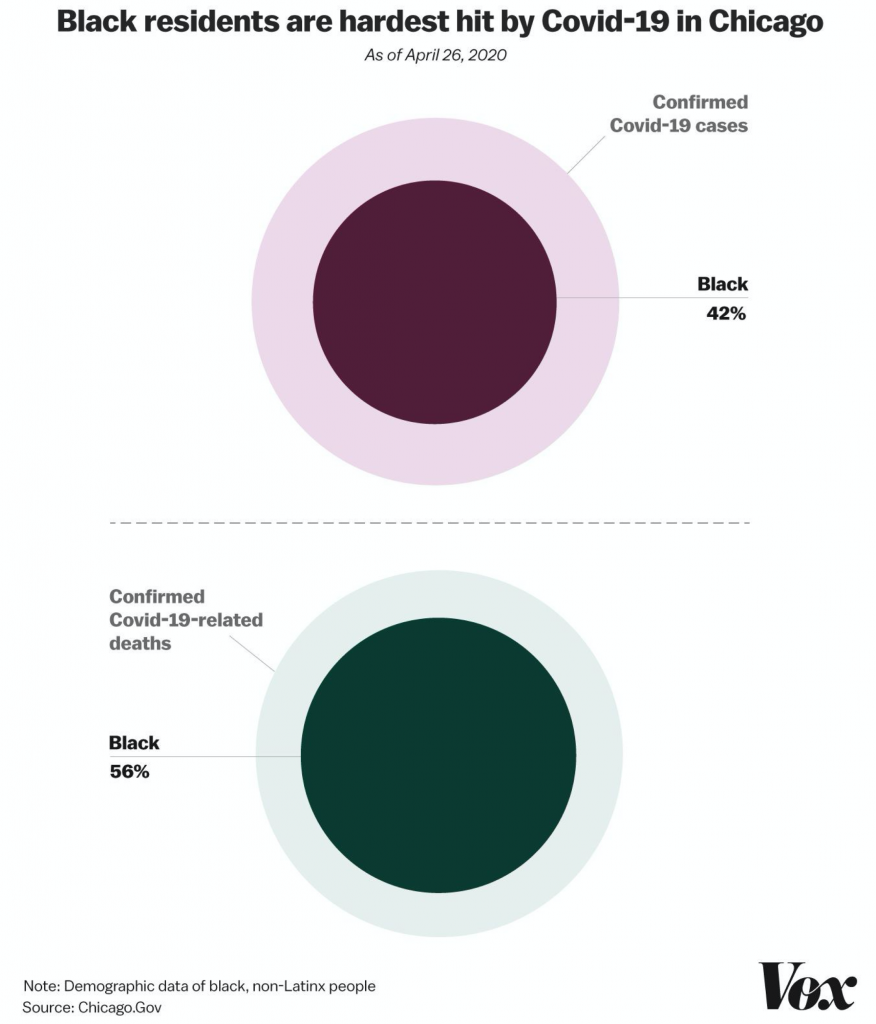
Yet for weeks, some black neighborhoods on the South Side of the city with the highest number of cases were tested at a lower rate than the whiter wealthy areas in the city center. It is a problem reflected statewide, and increasingly nationwide. Available data from the state of Illinois shows that even though black residents make up 37 percent of the state’s Covid-19 deaths, they only received 13 percent of the state’s tests, as of April 23.
It wasn’t supposed to be this way. Chicago serves as the model city of what the White House christened a month ago as an “extraordinary” and “historic” public-private partnership to offer free, accessible coronavirus testing across the country at retail pharmacies and grocery stores.
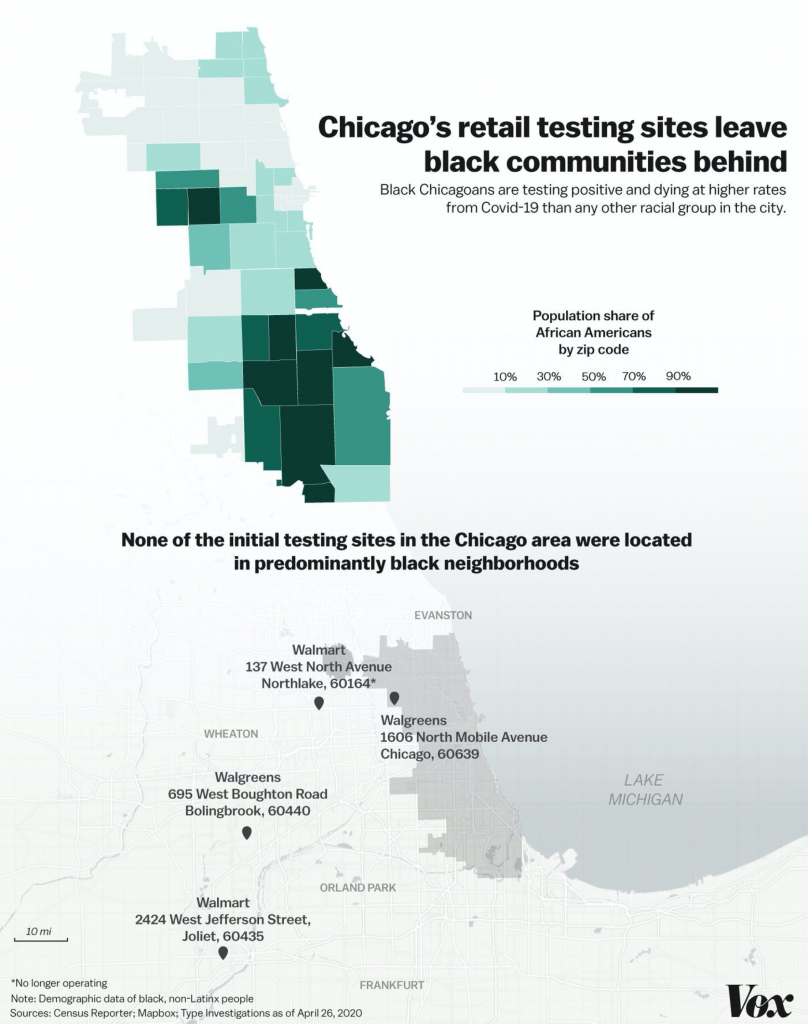
With three current sites (one recently closed), the Chicago area is among cities with the most retail testing sites in the nation. But a Type Investigations and Vox analysis shows the sites are largely inaccessible for residents in the hardest-hit areas: the city’s predominantly black neighborhoods. The closest retail drive-through testing site to Adarra is at least 18 miles away.
At a press conference on Monday, President Trump touted the testing program, saying, “These private sector leaders along with others have been exceptional partners in an unprecedented drive to expand the states’ capabilities and our country’s capabilities.”
But more than a month after the program’s debut, the sluggish rollout and locations of the retail drive-throughs participating in the White House’s partnership have left cities and states scrambling to find solutions for testing, especially in majority-minority neighborhoods, where residents of color have been disproportionately impacted by the pandemic.
The Trump administration promised widespread, retail-based testing, but the rollout was slow. Black communities have been devastated.
On March 13, the Trump administration announced its partnership with Walgreens, Walmart, Target, and CVS to provide a portion of their parking lots across the nation for free drive-through testing. The administration asserted that the plan would “meet the needs of the American public,” with Trump emphasizing that “we have many, many locations” and that “we cover very, very strongly our country — stores in virtually every location.”
White House coronavirus response coordinator Dr. Deborah Birx said the plan was expected to be so efficient that after scaling across the United States, “we want to bring this across the continent.” Moreover, partner stores professed a focus on the hardest-hit communities. Walgreens declared testing would focus on “our most vulnerable citizens,” and CVS said it would scale to quickly serve “the most vulnerable members of our communities.” The stock market rallied after the announcement. Rite Aid and Kroger joined the effort soon after.
Yet the ambition of this project is overshadowed by its failures, as Covid-19 infections increased exponentially in America’s urban centers. As of April 16, there were only 17 retail locations open. (Just a few days prior, on the 13th, NPR characterized retail drive-through testing as “largely nonexistent.” ) All of those stores, save three, are located in predominantly white areas. Between April 17 and 27, 43 more retail testing sites opened, but only five of those are in predominantly black areas.
A Health and Human Services spokesperson said the department is working with pharmacy and retail companies to “expand rapidly to areas that are under-tested and socially vulnerable” and that the department is “using data to locate sites in counties that are under-tested and socially vulnerable, especially those with high populations of black, Hispanic and rural Americans.” They noted that “as of April 24, 63 sites are testing Americans in 24 states.”
However, of the 63 testing sites operating, or announced to open as of April 24, only eight — about 13 percent — are in predominantly black neighborhoods. Black Americans make up 30 percent of Covid-19 patients, according to preliminary nationwide data from the Centers for Disease Control and Prevention.
On the South Side of Chicago, the heart of the city’s black community, the retail testing centers are essentially a nonfactor. After watching the president’s store-based testing announcement, Illinois state Sen. Robert Peters said “it came off like this is more about highlighting all these people in this business space with no real concrete plan — it’s a pipe dream.”
Peters is one of the many black politicians and activists who, in recent weeks, have pushed for a South Side testing center to fill the gaps. Accessible testing is needed on the West Side, too. This month, Illinois state representative and board member of Loretto Hospital LaShawn K. Ford joined in a press conference outside Loretto to decry the lack of testing in the West Side community of Austin, Chicago, where about 80 percent of residents are African American.
“On the West Side of Chicago, the demand for testing is very high, and the supply is very minimal — that’s the problem,” Ford said. “When we hear the governor of Illinois and the president of the United States talk about bending the curve, what we’re going to find is we really can’t talk about raw numbers when we’re not testing a large segment of our population, and that’s the black community. There are no major test sites in the black community.” (One initial retail site is in the city limits, in a neighborhood adjacent to Austin but not predominantly black.)

Ford said he’s been under pressure from his constituents, who are “frustrated because they see other communities with these huge test sites set up by the government, and Walmart, and other facilities with big drive-ups. Yet a large segment of the population is ignored. And it’s been recently noted that the segment that has been ignored is the segment that’s been the hardest hit with deaths and positive cases.”
According to public data, black Chicago residents are dying of Covid-19 at four times the rate of white residents. Statewide, black Illinoisans are testing positive at twice the rate of their white counterparts. All the while, black Illinoisans have received about half as many tests.
A retail-based testing plan leaves communities of color behind
Assessing the White House retail testing plan from its inception, Rutgers professor Naa Oyo A. Kwate argues that centering stores as testing points compounds issues of access because of retailers’ segregated location patterns, generally away from black neighborhoods.
Kwate said a more equitable option could have been chosen, such as post office parking lots or schools, which are more equally distributed throughout communities. “Trying to respond to the pandemic by partnering with private retail sites, that doesn’t really make sense,” said Kwate, adding that the few testing centers in the Chicago area aren’t strategically located relative to the population density and the city’s hardest-hit communities.
With half of the Chicago region’s retail testing centers at a Walgreens and Walmart in far-flung suburbs, Kwate said, “if you’re on either on the South Side or in a predominantly black suburb, you have to go a really long way — you’re driving on the expressway for at least half an hour, paying tolls to get there. It’s nowhere close to where you are.”
Struggles with the White House’s rollout of its retail plan have been coupled with rhetorical efforts to shift responsibility and blame. Initially, the White House took the lead. On March 13, standing in the Rose Garden alongside store CEOs, White House officials described retailers playing an integral role in the coronavirus task force’s “new partnership with the private sector to vastly increase and accelerate our capacity to test for the coronavirus.”
Later, stores reinforced the White House and federal government’s leadership role. CVS noted that “we are partnering with the federal government to support this effort,” and Walgreens announced that locations had been chosen “in collaboration with the U.S. Department of Health and Human Services.”
According to reporting from the Chicago Tribune, Walmart’s testing centers in the Chicago area were “privately managed under federal contracts.” Yet despite the federal government announcing the retail plan, choosing the retail locations, and managing the retail contracts, the president placed the onus of shortcomings on the states.
On April 14, after reports of sputters in retail testing, Trump distanced himself from the plan. He asserted that if states wanted retail testing centers, they should find a way to direct it themselves. “Washington shouldn’t be doing that,” Trump said during a briefing. “We can’t be thinking about a Walmart parking lot that’s 2,000 miles away where we’re doing testing, but a governor of a state can, and a mayor can, and right down the line.”
The next day, Trump once again framed the initiative as a responsibility of state governors and companies, and threatened to punish these local leaders if they poorly implemented it. Asked when retail testing would be broadly available to more Americans, Trump replied that “the companies will determine that, and the governors will determine that,” adding, “if we’re not happy, we’ll take very strong action against a state or a governor.”
Explaining why the public-private partnership has not reached a wider scale, reports in Business Insider and the Washington Post cited retailers’ struggle to gain access to enough tests and testing materials, and manage the large demand.
The White House addressed concerns of scale and equity in a recent press briefing. “I want you to know that we’re building on the public-private partnership that the president rolled out with pharmacy and retail companies like CVS, Walgreens, Rite Aid, and Kroger to accelerate testing for more Americans in more communities across the nation. We’re going to be increasing access to testing for undertested, underserved, and minority communities,” said Surgeon General Jerome Adams last Wednesday, mentioning companies that have joined the effort since the initial announcement.
Amid federal dysfunction, under pressure from advocacy groups and politicians, and in light of emerging racial disparities, many governors have moved to fill the void of the president’s testing plan in minority neighborhoods. This month, Illinois Gov. J.B. Pritzker announced that he would be launching new testing centers in black communities. Louisiana Gov. John Bel Edwards said he would be doing the same in rural areas. New York Gov. Andrew Cuomo announced his administration would provide pop-up testing sites in “minority communities downstate” in New York City. And partnering with the Urban League, Florida recently opened walk-up centers to reach black communities in Broward County.
The market-based failure resonates with black Americans
The White House’s inability to facilitate widespread free public testing through private sector retailers fits within a broader critique of the administration’s market-based response to the coronavirus.
Earlier this month, New York Times Magazine writer Nikole Hannah-Jones criticized the posture, tweeting, “I never want to hear that the government should be run like a business. This crisis has laid bare the dangers of gutting our public institutions & services, depending on companies dedicated to profit rather than government-mandated to work for the common good. Death is the result.” The Times editorial board expressed similar sentiments, describing the White House coronavirus response as an “embrace of markets so extreme it might seem farcical if it wasn’t resulting in unnecessary deaths.”
The market-based failure resonates particularly for black Americans, who have previously suffered under marquee failed federal public-private partnerships. In her book Race for Profit, Keeanga-Yamahtta Taylor explores how reliance on private sector solutions to provide access to services like housing has traditionally left black communities woefully underserved.
“There is a reason why African American organizations, community groups, have always called for a greater role of the state, because of the ways that racism and discrimination run rampant and unchecked in the private sector,” Taylor said last year in an interview with Chris Hayes.
Moving forward, establishing a national coronavirus testing plan remains crucial for both managing spread and tracking inequity. This month, medical professionals continue to criticize the racial disparities in testing, particularly among African Americans. Though Trump has been reluctant to engage on testing failures, he has acknowledged Covid-19’s impact on African Americans has “been disproportional.”
Yet as retailers like CVS and Walmart continue to slowly scale up, they are facing problems in reaching people without access to cars, or who live in segregated neighborhoods where these stores are not as accessible. The Trump administration has long opposed the consideration of disparate impacts in policymaking. It remains to be seen whether the federal government will be able to implement a testing system to fully address the racial inequities — and stymie the coronavirus’s disparate impact on black Americans.
This article was reported in partnership with Type Investigations.
Correction, April 28: An earlier version of this article misstated Adarra Benjamin’s job title, and a graphic misstated the number of deaths for certain demographic groups.
CREDITS
Type Investigations
Reporting editor: Alissa Figueroa
Data editor: Taylor Eldridge
Fact-checker: Hannah Beckler
Vox
Story editor: Kay Steiger
Graphics: Christina Animashaun
Photographer: Olivia Obineme for Vox
Visuals editor: Kainaz Amaria
Copy editors: Tim Williams and Tanya Pai