The coronavirus pandemic has had both economic and health care-related effects on the U.S.
The Centers for Disease Control and Prevention (CDC)’s Social Vulnerability Index (SVI) used U.S. Census Data to calculate which communities in the U.S. are particularly vulnerable when it comes to preparing for hazards, recovering from disaster, and other external stresses on human health. Factors include socioeconomic status, housing composition and disability, minority status and language, and housing type and transportation.
“What we’re seeing with coronavirus is it’s really exposing a range of longstanding underlying disparities in health care access, in health care outcomes, as well as in social and economic factors across communities,” Samantha Artiga, director of the Disparities Policy Project at the Kaiser Family Foundation, told Yahoo Finance.
And as U.S. states start re-opening amid the outbreak, the SVI data could provide extra context to issues like costs of coronavirus treatment, coverage gaps (particularly in rural areas), and how minorities are being disproportionately affected by the virus compared to their white counterparts.
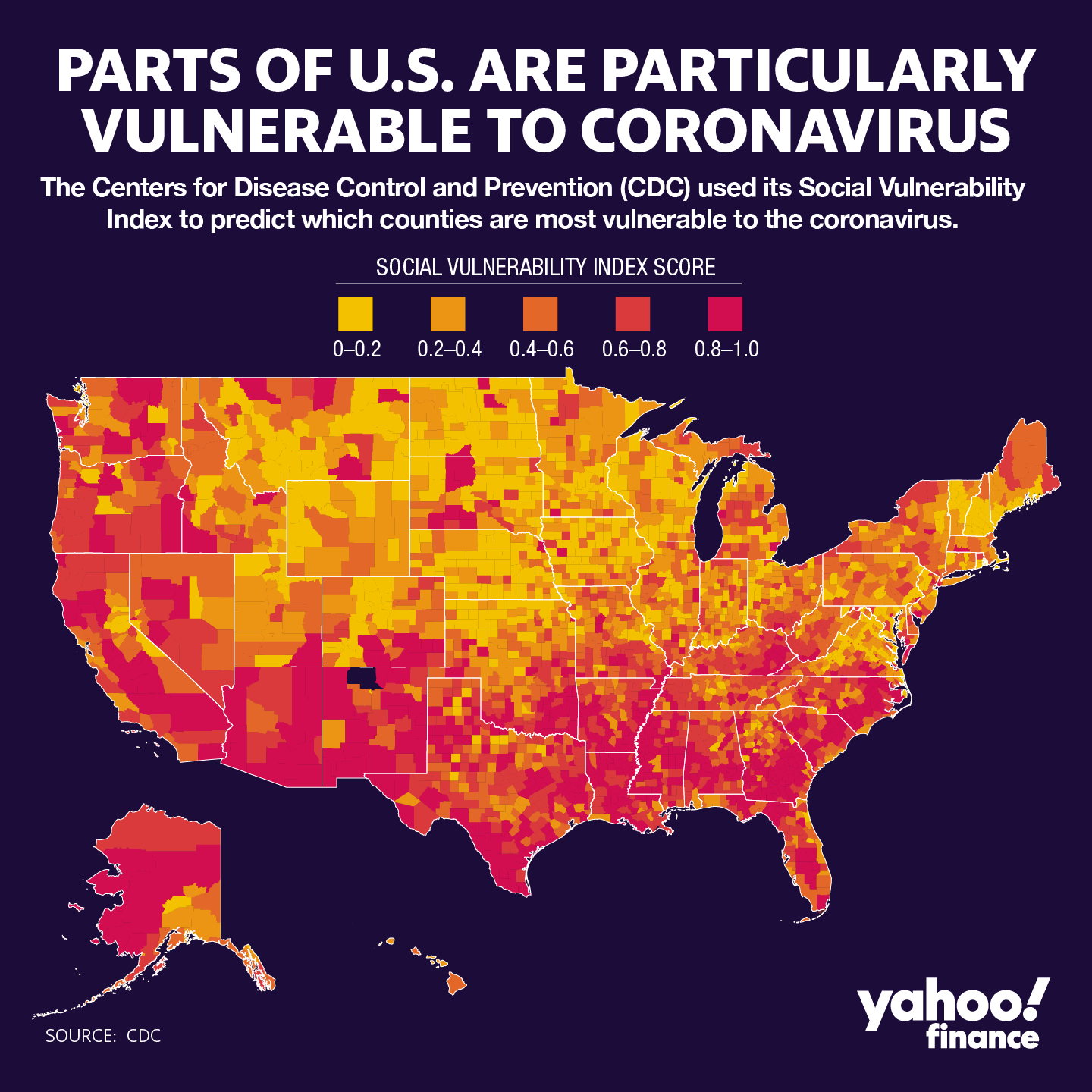
Why the South is vulnerable
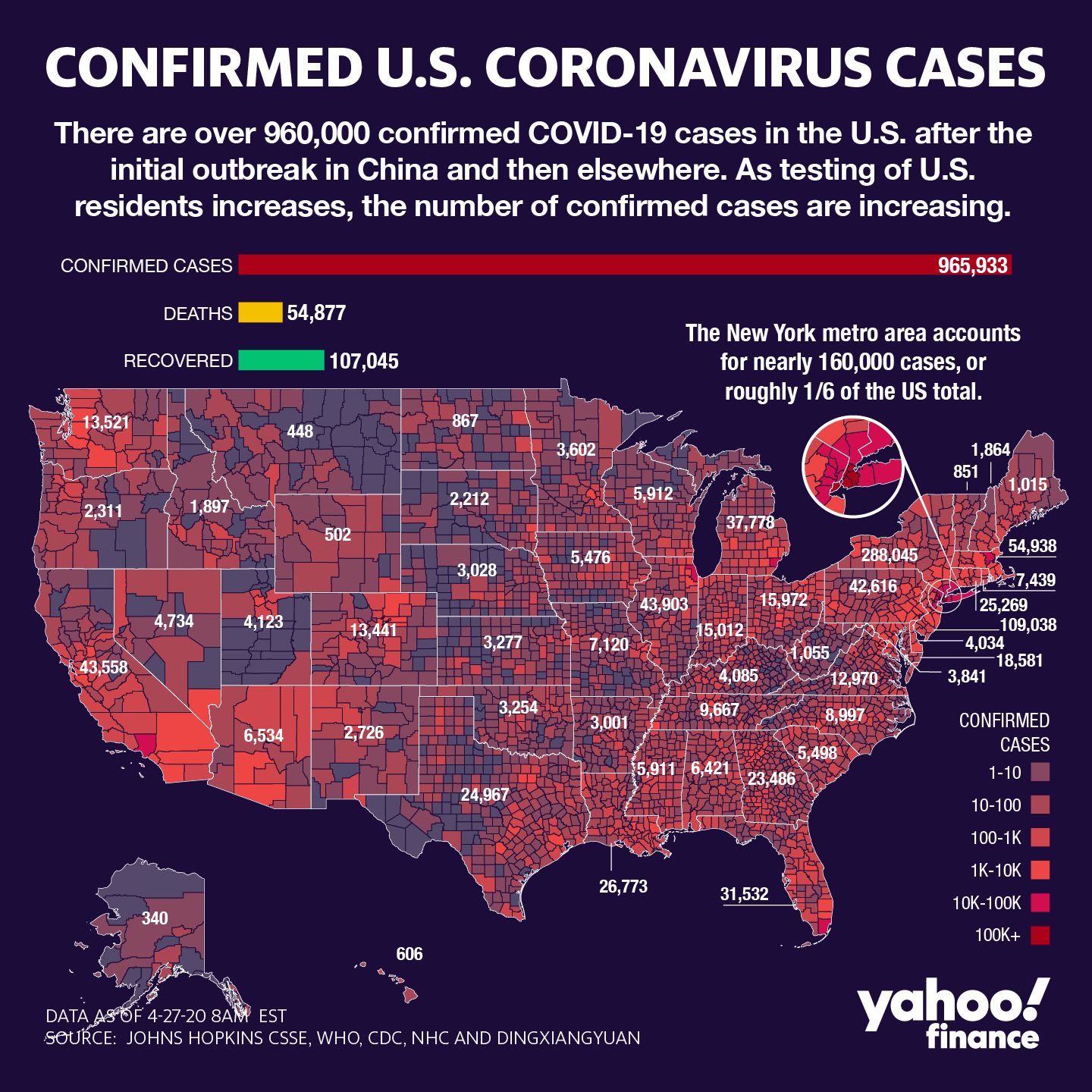
The coronavirus has swept its way across the U.S. since the first confirmed casewas reported in the country on January 20, 2020.
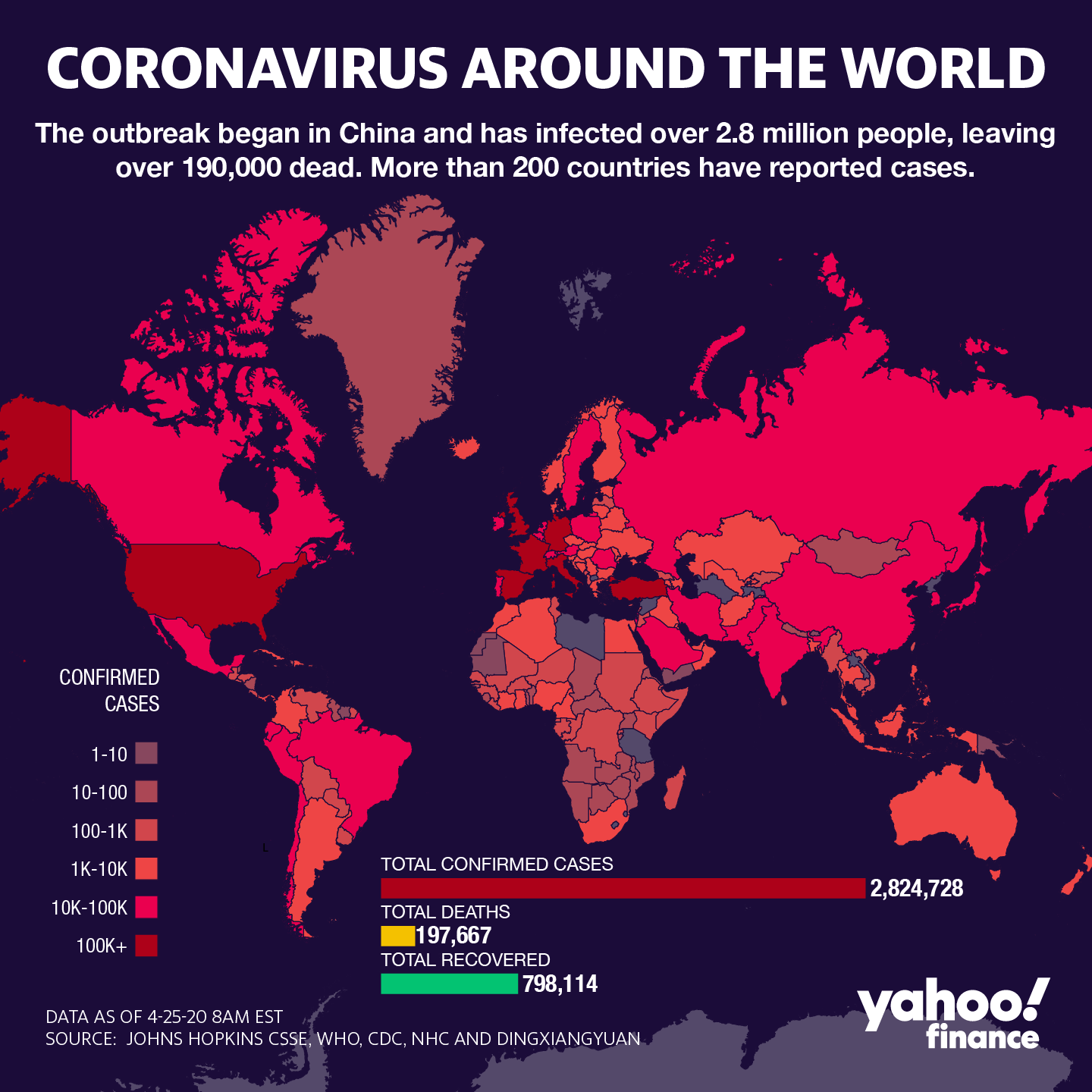
Since then, nearly 1 million Americans have been confirmed to have the coronavirus, making the U.S. the global leader in case count. Worldwide, there are over 2.8 million cases.  112 PHOTOSCoronavirus in the United StatesSEE GALLERY
112 PHOTOSCoronavirus in the United StatesSEE GALLERY
At this point, a majority of states have implemented stay-at-home orders to try to contain the spread of the virus and limit travel to only essential tasks. Nevertheless, some parts of the country have significantly been hit harder than others in terms of coronavirus cases.
“If you look regionally across the country, particularly in the South, there are higher rates of chronic conditions,” Artiga said. “And there’s more limited access to health insurance coverage because a number of states in the South haven’t adopted the Affordable Care Act Medicaid expansion.”
Although New York City is the national epicenter of the coronavirus, other U.S. hot spots include New Orleans, the greater Houston area, and the greater Atlanta area, and parts of Florida. Louisiana did adopt and implement Medicaid expansion, but the other three states did not.
‘An individual’s health is reflective of an array of different factors’
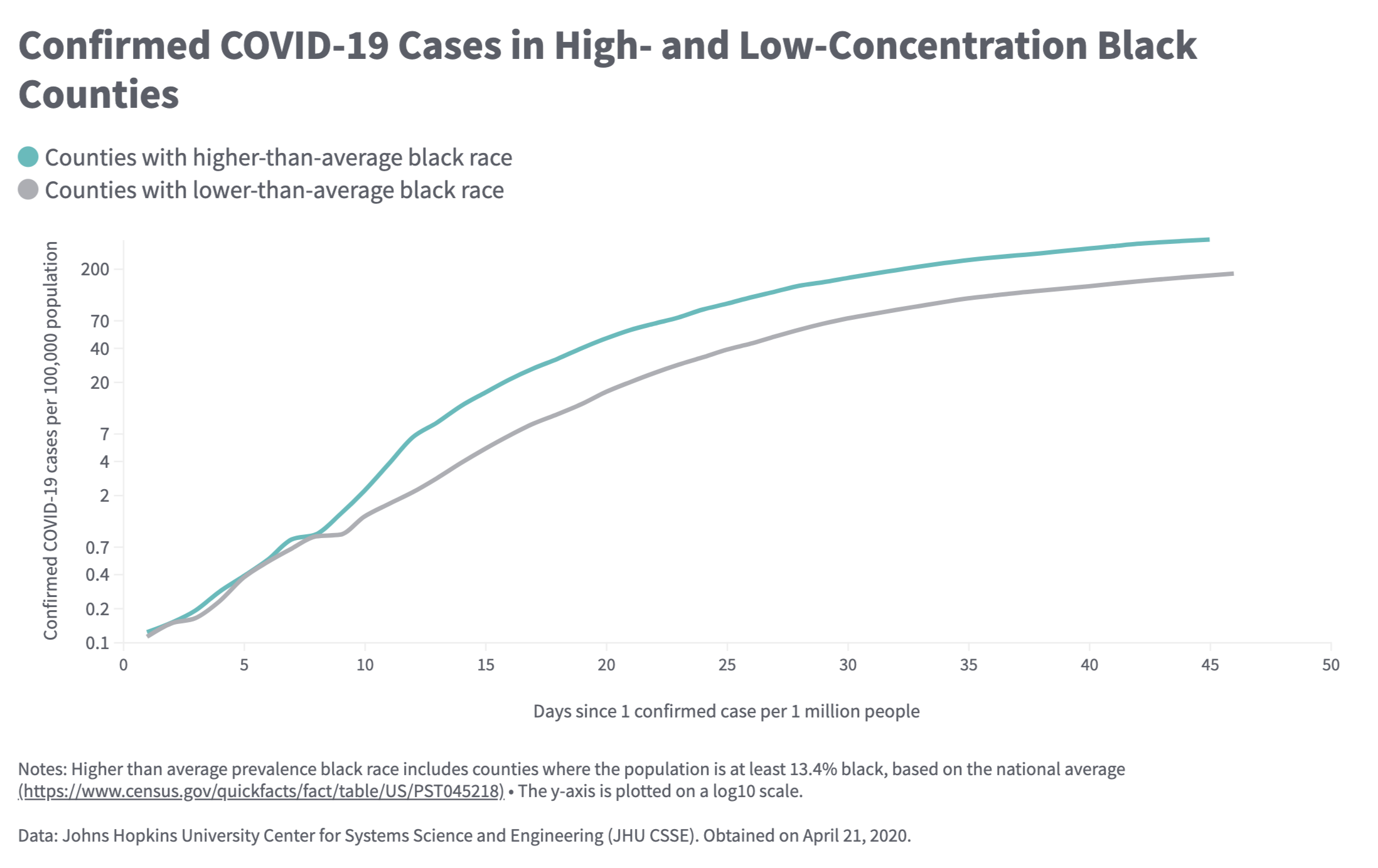
Race is another factor at play.
Majority-black counties are three times more likely to have coronavirus cases and have almost six times the death rate as white-majority counties. In Louisiana, in particular, 70% of more than 1,600 coronavirus fatalities are African Americans, even though they are just 32% of the state’s population.
Chronic diseases are one part of it. And according to Artiga, it’s tied to underlying disparities in health care access and other socioeconomic factors.
“Particularly over the past few years,” she said, “there has been growing recognition that an individual’s health is reflective of an array of different factors, including the extent to which their ability is to access health care, but also a range of socioeconomic factors: Do they have access to nutritious food? What are their transportation options? What is their housing situation? What is their job? What is their income? All those factors will influence an individual’s health.”
Congresswoman Ayanna Pressley (D-MA) recently made a similar argument on Twitter:
A report from the Commonwealth Fund corroborated that notion, finding that counties with large black populations have faced higher case counts of coronavirus, higher mortality, and a faster pace of progression compared to counties with low black populations.
“By April 21, high-concentration black communities saw 422,184 confirmed COVID-19 cases and 27,354 deaths, compared to 378,667 cases and 16,203 deaths in low-concentration black counties,” the report stated, adding: “The 681 high-concentration black counties account for only about a third of the U.S. population but 53% of the cases and 63% of the deaths nationally.”
Housing inequality becoming other kinds of inequalities
Andre Perry, a Brookings fellow and author of the forthcoming book “Know Your Price,” described structural inequality as a pre-existing condition.
“I would certainly say there are food deserts and other things, but understand housing inequality becomes other kinds of inequalities in our city, how they dictate so much of our lives,” Perry told Yahoo Finance. “When you don’t have affordability, you have overcrowding, you have worse conditions, you have predatory landlords.”
He continued: “What we’re finding is that wherever there are things like housing devaluation, poverty, high occupancy homes — those are the areas where your people are more vulnerable and they happen to be areas, not surprisingly, that are blacker. You’ve seen where black people live in the South and where there are concentrated areas of poverty, where there’s a lack of affordable housing, forcing people to live in intergenerational families or live intergenerationally in a household, those are the areas that are susceptible.”

‘COVID will go away, but the structural inequalities will persist’
Income inequality may be the largest underlying issue when it comes to coronavirus vulnerability.
A 2019 survey found that more than half of American renters have delayed medical care in order to pay rent. And 1 in 4 Americans have postponed medical care due to cost. This can lead to developing health conditions down the line, and leave them more susceptible to the coronavirus.
“Lower-income individuals are more likely to be uninsured because they’re more likely to work in jobs and occupations that may not offer health insurance coverage to their workers,” Artiga said, “or if health insurance is offered, they may not be able to afford the employee share associated with that.”
And while many Americans flocked to supermarkets to stock up on supplies when coronavirus cases began rising in the U.S., low-wage workers were more likely to struggle with buying two weeks worth of supplies. And for those who live in urban neighborhoods where corner stores and bodegas are the main sources of groceries, it’s difficult to buy in bulk since there are only small portions of each item.
“We’ve got to recognize that COVID will go away, but the structural inequalities will persist,” Perry said. “And if we don’t address the structural inequality while working on the emergency or the acute issues, black and brown people, we’ll be right back in the same position when the next crisis hits.”
Adriana is a reporter and editor for Yahoo Finance. Follow her on Twitter @adrianambells.




