Depression is a main cause behind poor health outcomes, according to the World Health Organization (WHO). Current research suggests that a staggering 300 million people across the globe struggle with depression. While depression doesn’t discriminate — it can happen to anyone, regardless of their age, gender identity, or race — marginalized racial groups feel the weight of this mood disorder the most. Recent studies reveal what many people already experientially know — black, indigenous, and people of color (BIPOC) are extremely affected by depression (via Everyday Health).
Additionally, a report published by the Blue Cross Blue Shield Association in May 2022 showed that among Black and Hispanic populations, depression is more likely not to be diagnosed — and as a result, many in these communities don’t receive the treatment they need. The causes of these racial disparities are multi-layered, resulting from a world and healthcare system deeply entrenched in racism. While anyone can have depression, BIPOC are hit the hardest and struggle to get back up due to racial inequities. The cycle is hard to break. Time and time again, science has linked racism to mental health disparities. As Wizdom Powell, chief social impact and diversity officer at Headspace Health and director of the Health Disparities Institute at UConn Health, stated in Everyday Health: “When white America catches a cold, all the other groups get the flu.”
If you or someone you know needs help with mental health, please contact theCrisis Text Line by texting HOME to 741741, call the National Alliance on Mental Illness helpline at 1-800-950-NAMI (6264), or visit the National Institute of Mental Health website.
Signs of depression

Prostock-studio/Shutterstock
Depression is a mental health disorder in which a persistent sense of disengagement and feeling of sadness can alter the way someone thinks, feels, and acts (via Mayo Clinic). This ultimately affects many aspects of life, from day-to-day activities and work to relationships and more. And through a domino-effect, depression can lead to a wide range of other issues, both physical and emotional. Signs of depression vary from person to person. However, the main symptoms include almost always feeling sad or without hope; lack of interest in things you used to love; changes in sleep, appetite, or weight; fatigue; lack of motivation; feelings of shame; cognitive difficulties, and other unexplained physical problems. Sometimes symptoms appear different in Black people and other marginalized communities because they may try to cover up or ignore their symptoms due to stigma or other concerns, like not being able to afford care (via Medical News Today). In addition, BIPOC may have a hard time accessing medical care to receive a diagnosis or treatment, so their symptoms might change, become more serious, or look different over time.
Complications of depression

Dragana Gordic/Shutterstock
The fact that depression goes undiagnosed and untreated at much higher rates in BIPOC communities means that these groups of people are also more susceptible to developing complications from depression. Signs of someone struggling with depression without help or treatment can take on many forms. For example, they might become overweight, which could lead to diabetes, heart disease, or other health issues over time. Or they may struggle with panic attacks or anxiety. Some might turn to drugs or alcohol to cope. Other serious complications of depression include cutting or self-mutilation and suicidal thoughts, attempting suicide, or committing suicide (via My Med).
The difficulties of depression go beyond the physical in intricate ways. Those struggling with depression are three times more likely to call in sick to work, and even more apt not to be able to hold a job at all (via Med Broadcast). The added financial burden of missing work or being unemployed can fuel stress and make healthcare unaffordable or unattainable, adding to the feelings of depression and further perpetuating the cycle. People suffering from depression also often have low self-esteem, which may affect their relationships with friends, family, coworkers, and loved ones, ultimately leading to feelings of isolation and loneliness.
If you or anyone you know is having suicidal thoughts, please call the National Suicide Prevention Lifeline by dialing 988 or by calling 1-800-273-TALK (8255).
BIPOC are more likely to develop serious symptoms and complications

Prostock-studio/Shutterstock
Overall, there are not many reliable studies that focus on how many BIPOC have depression. Some research has found that depression rates are about equal between white people and BIPOC, while others suggest that BIPOC are either less likely or more likely, to experience depression than white people (via Everyday Health). While the exact numbers aren’t confirmed, research reveals a trend — that BIPOC who develop depression are hit the hardest. BIPOC are more likely to develop severe symptoms and chronic complications of depression, making the mood disorder extremely hard to get out from under. “What this means is the burden of disability from depression is much more pronounced in individuals from Black, indigenous, and communities of color,” says Dr. Wizdom Powell, chief social impact and diversity officer at Headspace Health, to Everyday Health. “And the consequences of these mental health conditions are far more significant and negative for these populations.”
Financial barriers

fizkes/Shutterstock
Money: one of the largest causes of mental health issues and one of the biggest barriers to receiving mental healthcare. Some of the risk factors for developing depression include race, socioeconomic standing, and employment status (via Neuropsychiatric Disease and Treatment). In the U.S., Black and Hispanic people experience poverty far more than white people. Unsurprisingly, poverty and low-income are linked to mental struggles — Black people who live below the poverty line have a more than doubled chance of having psychological stress (via Everyday Health). And research has established that living in poverty is a barrier to mental healthcare. Mental healthcare, including therapy and medication, is expensive. If you’re low-income or unemployed, treatment may not be an option. The top reason people across all racial groups do not utilize mental healthcare is a lack of health insurance or the high cost of care (via Bennett College). In 2020, more than 10% of Black people in America did not have health insurance.
BIPOC are more likely to experience poverty, and systemic racism is a key cause. One example is the Black-White wealth gap that exists due to historic and continuing discrimination in employment opportunities and mortgage eligibility, among other issues. According to the Center for American Progress, “From slavery to Jim Crow, from redlining to school segregation, and from mass incarceration to environmental racism, policies have consistently impeded or inhibited African Americans from having access to opportunities to realize the American dream.”
Racial disparities in treatment

Kmpzzz/Shutterstock
BIPOC are underdiagnosed for depression, in part due to the shortcomings of medical providers — according to a recent research review, some medical professionals are unable to recognize the symptoms of depression in BIPOC. There are two theories of this phenomenon: the “clinician bias” hypothesis and “cultural relativity.” The “clinician bias” theory holds that medical professionals gauge people from each race differently despite believing that symptoms present similarly across racial lines. The “cultural relativity” theory is based on the idea that depression manifests differently in different racial groups, but a doctor may be inconsiderate or unaware of these cultural differences.
“Implicit racial bias” occurs when a clinician’s assumption about a certain individual based on their race can unknowingly result in treating them differently(via Justice Research and Statistics Association). When it comes down to it, doctors are human and humans make mistakes, especially because they exist in a society that is steeped in systemic racism (via Health Affairs). Even if a doctor is anti-racist and aware of the potential for these biases, they may still unwittingly act upon bias — systemic racism is so embedded in our society that oftentimes it appears in subtle ways on a subconscious level (via the American College of Cardiology).
The stigma of depression

Prostock-studio/Shutterstock
Mental health stigma exists everywhere: For instance, you may have heard phrases like “boys don’t cry,” “suck it up,” “you’re being hysterical,” or “just get over it.” A stigma is formed when someone has a negative perception of an individual based on some particular quality about that person, such as that they have a mental illness (via Everyday Health). Stigma can also be self-made — someone with depression may feel ashamed or wrongly assume they should be able to control it or they’re a failure (via Mayo Clinic). Misunderstandings and a lack of education are key factors behind the stigma.
The stigma of depression can stop anyone from seeking care, regardless of race. But some studies reveal that mental health stigma is heavily experienced in Black communities (via Medical News Today). Research has found that many Black people see depression as a sign of weakness, and that this stigma can stop those with depression from admitting they have mental health issues and seeking treatment. This type of mental health stigma is also seen in Hispanic and Latino communities, with many people avoiding talking about the topic of mental health problems in general because it’s considered “taboo” (via Everyday Health). These stigmas stop people from getting the important help they need.
Racism and racial disparities in healthcare settings

Prostock-studio/Shutterstock
Many BIPOC can be hesitant to seek medical care, for a variety of reasons. For instance, more than half of Black Americans report a lack of trust in the healthcare system, with a fifth noting that they’d had a previous bad experience due to racism (per Andscape). And mistrust in the medical establishment is understandable given that historically, BIPOC have been used as unconsenting test subjects in healthcare settings. One horrifying example that fuels this skepticism is seen in the U.S. Public Health Service (USPHS) Syphilis Study at Tuskegee. From 1932 to 1972, the USPHS deliberately withheld treatment in nearly 400 Black men who had syphilis. The patients didn’t know what the study was about or that they even had syphilis (via Everyday Health). As a result, over a quarter of the men died, and a number of their wives and children were infected.
Additionally, BIPOC might struggle to find mental health professionals who are not white, and who may more accurately understand their experiences (via HelpGuide). The lack of diversity in the medical field can have a meaningful effect: Research confirms that when a doctor and patient share the same race, the patient is more likely to open up to their physician and to follow testing and treatment recommendations (via University of Michigan Medicine).
Stress from racism deepens depression
Lightspring/Shutterstock
Let’s state the obvious: Stress caused by racism increases the risk of depression. Stress and stressful life events have long been linked with depression (via Neuropsychiatric Disease and Treatment). And according to an analysis of almost 300 studies published between 1983 and 2013, racism was connected to mental health issues including depression, anxiety, psychological stress and other problems (per PLoS One). Indeed, Black people have a higher chance of experiencing depression due to racism (via Medical News Today). There are many ways BIPOC experience race-related stress, including personal experiences of discrimination or systemic racism, secondhand stories of racism (such as the murder of George Floyd), and micro-aggressions, just to name a few (via Chicago Psychotherapy). Over time, this chronic stress from racial discrimination can lead to hyper-vigilance — BIPOC who experience racism become conditioned to be on guard for future types of discrimination. Therefore, “BIPOC individuals in a systemically racist society are often continuously experiencing a heightened stress response — consciously or unconsciously — which has direct effects on both physical and psychological well-being over time,” according to Chicago Psychotherapy.
Generational trauma

Josep Suria/Shutterstock
The concept of generational trauma, or intergenerational trauma, explains how a collection of negative past experiences from previous ancestors can show up in your DNA (via Bennett College). It’s based on a new field of science known as epigenetics, which studies how environmental events experienced by your parents and other relatives can impact your genes. Research suggests that BIPOC communities are affected by significant levels of generational trauma due to centuries of persistent oppression, violence, discrimination, and racism (via Healthline). Other potential causes include war, genocide, slavery, natural disaster, poverty, and so much more. Generational trauma was first brought to light after researchers noticed significant mental health struggles experienced in the descendants of Holocaust survivors.
The signs of generational trauma can manifest in many ways and vary across individuals — some even mirror the symptoms of depression and post-traumatic stress disorder (PTSD). Signs someone is experiencing generational trauma include dissociation, disconnection, apathy, loneliness, withdrawal, insecurity, hyper-reactivity to stress, low self-esteem, and feelings of helplessness, anxiety, and depression.
Chronic health conditions and depression

venusvi/Shutterstock
Chronic health conditions seemingly affect almost every aspect of life, depending on the condition. Arthritis can make everyday activities difficult, and cancer, heart disease, and diabetes can lead to life-threatening complications (via Department of Health). About a third of those with chronic health issues also have depression (via WebMD). A multitude of factors — including racial disparities in healthcare, but also issues of systemic racism like exposure to lead or toxins, living near air pollution, poverty, barriers to education, or unavailability of fresh foods — mean that BIPOC populations have higher rates of the kinds of chronic conditions that can be comorbid with depression (per WebMD).
The chances of BIPOC developing a chronic health issue is as much as double that of a white person. These multi-layered factors, often referred to as social determinants of health, are to blame — not biology. “It’s really important to make that distinction. We have no evidence that certain groups are biologically inclined to have more chronic disease. But what we do see are patterns by race and ethnicity,” Natalia Linos, executive director of the FXB Center for Health and Human Rights at Harvard University, told WebMD. The weight of depression is heavy — but when you stack other chronic health conditions on top of it, the burden becomes compounded, as each illness comes with its own set of far-reaching physical, emotional, and financial side effects (via the National Institute of Mental Health).
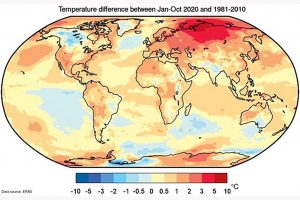
Climate inequities and depression
Triff/Shutterstock
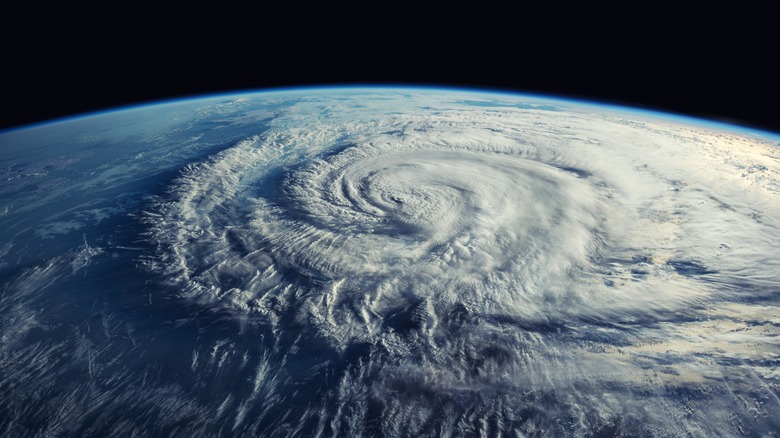
Climate change is happening, and it’s here to stay (via BBC News). Extreme weather due to climate change is impacting people worldwide, causing heatwaves, droughts, massive floods, wildfires, landslides, and more. Emerging research confirms that climate change is causing mental health issues as a consequence of the stress and trauma of enduring these severe weather patterns. According to a 2021 report by the American Psychological Association, ecoAmerica, and Climate for Health, systemic racism and discrimination combined with being subjected to climate effects can cause many mental health issues like stress, anxiety, depression, mood disorders, PTSD, and more. The report emphasizes that marginalized communities are also impacted by climate change the most.
There are many complex causes for this. First, minority groups are already more vulnerable to climate change impacts due to factors such as inequity, poverty, stolen land, and malnutrition. Marginalized communities are also more likely to be exposed to environmental pollution — for example, one study found that white neighborhoods in England and The Netherlands have less air pollution than BIPOC neighborhoods. This phenomenon has also been documented with the recent heatwaves experienced worldwide — marginalized neighborhoods are noticeably several degrees warmer than other surrounding neighborhoods (via Prevention Web). Dubbed the “urban heat island” effect, this has been attributed to the fact that these areas have more concrete and fewer trees and parks, and consequently less shade.
Food deserts and depression

Black Salmon/Shutterstock
Poverty and hunger go hand in hand. As BIPOC face higher rates of low-income wages and unemployment, it becomes increasingly difficult to put food on the table (via Economic Policy Institute). Indeed, Black or Hispanic households face food insecurity at double the rate of white households, according to data from 2001 to 2016 (via Family and Community Health). The impacts of food insecurity on a family — especially one with children — include a higher risk of certain chronic health issues; depression in mothers in particular; and stunted development, behavioral issues, and lowered academic performance in children. According to a recent study, food insecurity dramatically increases — by a magnitude of about 250% — someone’s chances of developing anxiety or depression (via BMC Public Health).
The term “food desert” describes an area that lacks access to high-quality and low-cost healthy food. Neighborhoods with a high number of minority groups are the most likely to be a food desert, according to 2012 report by the United States Department of Agriculture (USDA). Food deserts also tend to be areas with higher levels of poverty and less reliable public transportation.
Gentrification

Catherine Zibo/Shutterstock
The word “gentrification” refers to a situation of neighborhood change and the subsequent displacement of low-income residents (via Mindpath Health). It occurs when richer people begin moving into a particular neighborhood, driving up residential and living costs to the point that previous residents can no longer afford to live there. This means that people who have lived in a neighborhood for a long time and formed connections with the community are displaced. The culture often also changes, as businesses in the area start to shift to serve the new residents. This can have a negative impact on the low-income or displaced residents, causing heightened levels of stress, depression, and other health issues. A recent scientific study that looked at displaced individuals in California confirms that gentrification contributes to mental health disparities. Gentrification also negatively impacts the mental health of children being displaced — one meta-analysis that examined low-income neighborhoods in New York City found that children between the ages of 9-11 experienced much higher levels of anxiety and depression due to gentrification compared to children of the same age group who lived in low-income neighborhoods that were not gentrified.
If you or someone you know needs help with mental health, please contact theCrisis Text Line by texting HOME to 741741, call the National Alliance on Mental Illness helpline at 1-800-950-NAMI (6264), or visit the National Institute of Mental Health website.